DNP 805 EHR Database and Data Management
Grand Canyon University DNP 805 EHR Database and Data Management– Step-By-Step Guide
This guide will demonstrate how to complete the Grand Canyon University DNP 805 EHR Database and Data Management assignment based on general principles of academic writing. Here, we will show you the A, B, Cs of completing an academic paper, irrespective of the instructions. After guiding you through what to do, the guide will leave one or two sample essays at the end to highlight the various sections discussed below.
How to Research and Prepare for DNP 805 EHR Database and Data Management
Whether one passes or fails an academic assignment such as the Grand Canyon University NUR 550 Benchmark – Evidence-Based Practice Project: Literature Review depends on the preparation done beforehand. The first thing to do once you receive an assignment is to quickly skim through the requirements. Once that is done, start going through the instructions one by one to clearly understand what the instructor wants. The most important thing here is to understand the required format—whether it is APA, MLA, Chicago, etc.
After understanding the requirements of the paper, the next phase is to gather relevant materials. The first place to start the research process is the weekly resources. Go through the resources provided in the instructions to determine which ones fit the assignment. After reviewing the provided resources, use the university library to search for additional resources. After gathering sufficient and necessary resources, you are now ready to start drafting your paper.
How to Write the Introduction for DNP 805 EHR Database and Data Management
The introduction for the Grand Canyon University DNP 805 EHR Database and Data Management is where you tell the instructor what your paper will encompass. In three to four statements, highlight the important points that will form the basis of your paper. Here, you can include statistics to show the importance of the topic you will be discussing. At the end of the introduction, write a clear purpose statement outlining what exactly will be contained in the paper. This statement will start with “The purpose of this paper…” and then proceed to outline the various sections of the instructions.
Need a high-quality paper urgently?
We can deliver within hours.
How to Write the Body for DNP 805 EHR Database and Data Management
After the introduction, move into the main part of the DNP 805 EHR Database and Data Management assignment, which is the body. Given that the paper you will be writing is not experimental, the way you organize the headings and subheadings of your paper is critically important. In some cases, you might have to use more subheadings to properly organize the assignment. The organization will depend on the rubric provided. Carefully examine the rubric, as it will contain all the detailed requirements of the assignment. Sometimes, the rubric will have information that the normal instructions lack.
Another important factor to consider at this point is how to do citations. In-text citations are fundamental as they support the arguments and points you make in the paper. At this point, the resources gathered at the beginning will come in handy. Integrating the ideas of the authors with your own will ensure that you produce a comprehensive paper. Also, follow the given citation format. In most cases, APA 7 is the preferred format for nursing assignments.
How to Write the Conclusion for DNP 805 EHR Database and Data Management
After completing the main sections, write the conclusion of your paper. The conclusion is a summary of the main points you made in your paper. However, you need to rewrite the points and not simply copy and paste them. By restating the points from each subheading, you will provide a nuanced overview of the assignment to the reader.
How to Format the References List for DNP 805 EHR Database and Data Management
The very last part of your paper involves listing the sources used in your paper. These sources should be listed in alphabetical order and double-spaced. Additionally, use a hanging indent for each source that appears in this list. Lastly, only the sources cited within the body of the paper should appear here.
Stuck? Let Us Help You
Completing assignments can sometimes be overwhelming, especially with the multitude of academic and personal responsibilities you may have. If you find yourself stuck or unsure at any point in the process, don’t hesitate to reach out for professional assistance. Our assignment writing services are designed to help you achieve your academic goals with ease.
Our team of experienced writers is well-versed in academic writing and familiar with the specific requirements of the DNP 805 EHR Database and Data Management assignment. We can provide you with personalized support, ensuring your assignment is well-researched, properly formatted, and thoroughly edited. Get a feel of the quality we guarantee – ORDER NOW.
Sample Answer for DNP 805 EHR Database and Data Management
Databases in the medical field provide a suitable framework for collecting, analyzing, and monitoring vital health information such as tests, expenditures, invoicing and transactions, patient information, etc. These records must be stored private from the general public while being widely available to health care providers who utilize them to save lives (Pastorino et al., 2019). This paper seeks to describe how a database can be used to diagnose chronic obstructive pulmonary disease (COPD) early diagnosis.
Clinically Based Patient Problem
COPD is a prevalent long-term condition marked by acute respiratory cough and shortness of breath, coughing, and sputum secretion. COPD is typically caused by prolonged exposure to hazardous chemicals and pollutants (Agarwal et al., 2022). Smoking accounts for approximately 85 percent of patients with COPD (Asamoah-Boaheng et al., 2022). Smoking is the leading cause of respiratory injury and asthma. COPD may also be caused by smoke inhalation from fuel combustion (Choi & Rhee, 2020). If the evidence is in the person’s private files, the caregiver may ignore it. When the problem exacerbates, non-smokers are usually diagnosed with COPD (Choi & Rhee, 2020). Exacerbation is defined by deteriorating health problems such as increasing dyspnea, continuous sneezing, and a change in the color of the sputum (Holmes & Murdoch, 2017). Exacerbations individuals incur higher healthcare expenditures, and certain drugs used in therapy, such as corticosteroids, have long-term negative consequences (Asamoah-Boaheng et al., 2022). COPD might also be caused by genetic anomalies, including severe hereditary impairment of alpha-1 antitrypsin (AATD) (Asamoah-Boaheng et al., 2022), which could be overlooked in large amounts of data.
Individuals have one of two phenotypes that vary in intensity: acute emphysema or bronchiolitis. COPD must be evaluated in individuals who have difficulty breathing, sputum secretion, or persistent cough (Agarwal et al., 2022). Nevertheless, there are various other diagnoses for COPD, such as anaemia, lung cancer, persistent asthma, etc. COPD is often associated with concurrent chronic conditions such as diabetes and obesity, both of which produce various COPD-related symptoms such as cough and shortness of breath (Choi & Rhee, 2020). This postpones the diagnosis of COPD. The best technique to verify COPD in a person is high-quality spirometry. Spirometry is recommended when COPD is detected, and for a non-smoker with associated conditions, spirometry may be performed when the disease has progressed. The slow symptom onset further distinguishes COPD, so an individual may fail to detect dyspnoea despite having chronic coughing, causing COPD diagnosis to be delayed.
Early diagnosis is important in establishing the appropriate treatment course considering the individual’s severity and phenotype. Early detection has been found to enhance treatment experience by lowering the incidence and frequency of flare-ups, lowering treatment costs, and preventing long-term adverse effects associated with pharmacological treatment (Asamoah-Boaheng et al., 2022). Hospitals also avoid wasting money owing to erroneous treatment (Choi & Rhee, 2020).
Conceptual Database Design
The healthcare database is the backbone of the electronic health record, holding a wealth of organized and unstructured user data (Pastorino et al., 2019). The database material will only be relevant in the earlier detection and successful management of COPD if the unorganized data is analyzed to provide data that can be put inside the predefined metadata. The intended patient result in building the healthcare database will be the early identification of COPD by giving the provider access to patient health information from the database, which will then be utilized to detect COPD. The database shall contain comprehensive and accurate information received from or entered at the various hospital settings where the person has been treated. The data must also be accurately evaluated and structured, making it easier to remove differential diagnoses and do COPD confirmation spirometry.
ALSO READ:
DNP 805 Week 5 Assignment_Telehealth
236131_DNP 805 Evaluation of Healthcare Technology
DNP 805 Week 7 assignment Presentation
DNP 805 Case Report Health Care Informatics
DNP-805A-Health Care Informatics
The data items needed to construct the database to facilitate early diagnosis of COPD are identified and categorized as unstructured or structured during the conceptual design stage. Whereas structured data from the EHR may be directly filled into the system, unstructured data from caregivers’ and doctors’ notes are processed using natural language technologies to make data sensible within the environment. The relational database will include a healthcare-specific guideline and a language processing technology. The natural language-specific guideline deconstructs unstructured format input to enable NLP creators to execute specialized natural language processing inspections, including detecting the presence of vague terms. The healthcare-specific benchmark will then seek the relevant healthcare words and record the proper information in the correct fields depending on the context of the NPL transcribers.
Thus far, the database executes conventional database operations. The registry will include a unique COPD risk area to aid early detection. Whenever health records are processed, all past respiratory illnesses will be recorded under the COPD risk area. This section will be filled with indicators such as a persistent cough, breathlessness, and sputum secretion. The space will be filled with debris and hazardous gases from the patient’s surroundings. COPD is distinguished by the slow onset of symptoms that may or may not occur concurrently. Initially, an individual may describe dyspnoea without other symptoms, which may be missed and linked to a concurrent condition. Nevertheless, the data will be saved in the database so that when the person experiences a new symptom, such as mucus production, and the nurse brings up their record, the COPD risk area will be updated with all the identified symptoms thus far leading to early diagnosis. If the facility has a CDSS connected to the database, the CDSS program will notify the physician of a possible COPD diagnosis.
Attributes and Data Entities
1. Patient Details
This entity is a personal identification; it is connected to all the other properties which provide this person’s profile in the medical setting. All of its characteristics are organized, and these traits are objective.
Attributes
- Name (Varchar)
- Gender (Boolean)
- Age (Int)
- Address (Varchar)
2. Health Status
The entity represents the patient’s medical history as evaluated by the physician. Because the physician’s assessment and perception of the consequences of the patient’s condition may differ, all of the qualities are unstructured.
Attributes
- BMI (Int)
- Height (Int)
- Weight (Int)
- Blood Pressure (Int)
Because data submitted into the database is not primarily utilized for the initial COPD diagnosis, the entities described below will include more than the given characteristics. On the other hand, the features indicated must be included in the COPD risk section if the risk exists.
4. Genetics
The entity has qualities that describe physical and genetic anomalies that may impact the likelihood of COPD.
Attributes
- Alpha-1 Antitrypsin Dysfunction (Boolean)
3. Environment
Identifies the patient’s regular surroundings, which may raise COPD risk.
- Second-hand smoking inhalation (Boolean)
- Use of biofuels (Boolean)
- Work-related toxic contact (Boolean)
6. Medical history
Specifies the health history and updates the COPD risk field with factors that elevate the chance of COPD.
- Smoking history (Varchar)
- Smoking Frequency (Varchar)
- Respiratory diseases (Varchar)
5. Signs and Symptoms
This entity explains the patient’s present symptoms and the rationale for the hospitalization. Every symptom is regarded as a separate feature. The following symptoms will be included in the COPD risk field:
- Severe cough
- Sputum secretion
- Dyspnoea
The logical data model architecture concerns data modeling, which specifies the link between the objects. Figure 1 below illustrates the general conceptual map for the proposed database.
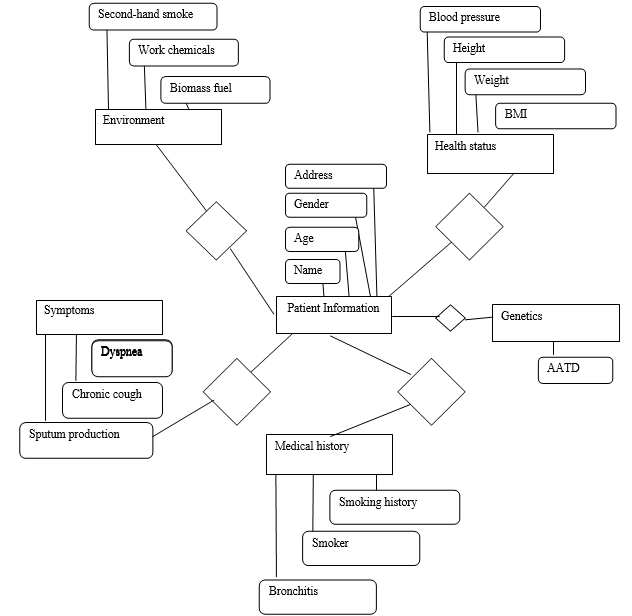
Figure 1: Conceptual map
Conclusion
The significance of a database in medical diagnosis cannot be ignored. It is critical for physicians, caregivers, and executive management to have timely and error-free access to detailed patient data. Hospital services rely on the efficiency, accuracy, and effectiveness of medical databases to ensure timely diagnosis and treatment, as in the case of COPD.
References
Agarwal, A. K., Raja, A., & Brown, B. D. (2022). Chronic Obstructive Pulmonary Disease. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK559281/
Asamoah-Boaheng, M., Farrell, J., Osei Bonsu, K., & Midodzi, W. K. (2022). Examining risk factors accelerating time-to-chronic obstructive pulmonary disease (Copd) diagnosis among asthma patients. COPD: Journal of Chronic Obstructive Pulmonary Disease, 19(1), 47–56. https://doi.org/10.1080/15412555.2021.2024159
Choi, J. Y., & Rhee, C. K. (2020). Diagnosis and treatment of early chronic obstructive lung disease(Copd). Journal of Clinical Medicine, 9(11), 3426. https://doi.org/10.3390/jcm9113426
Pastorino, R., De Vito, C., Migliara, G., Glocker, K., Binenbaum, I., Ricciardi, W., & Boccia, S. (2019). Benefits and challenges of Big Data in healthcare: An overview of the European initiatives. European Journal of Public Health, 29(Supplement_3), 23–27. https://doi.org/10.1093/eurpub/ckz168
Sample Answer 2 for DNP 805 EHR Database and Data Management
The adoption of information technology and reforms aimed at expanding access to healthcare services has led to the generation and accumulation of huge amounts of data by health care systems and organizations from multiple sources. The meaningful use incentive for utilization of the electronic health records (EHRs) has created vast and efficient data storage and databases that healthcare systems and providers can use to manage some of the common conditions affecting populations across the care continuum (Kruse et al., 2018). The purpose of this assignment is to discuss HER databases and management of data by focusing on a patient problem of surgical site infection. The paper explains incorporation of the information required to manage the issue, data required so that the database can manage the condition and enhance patient outcomes. The paper also describes entities that will be pulled from the EHRs and their relationships that the hypothetical database.
Patient Clinical Problem
The clinical issue of focus entails adult patients undergoing surgical procedure for colorectal cancer and susceptible to surgical site infections. According to Li et al. (2018), individuals undergoing colorectal cancer surgery have increased risk for morbidity (20%-40%) and mortality about 2% caused primarily by postoperative surgical site infections. Reports suggest that the rate of surgical infections has increased by over 25% in patients having a colon surgery (Grundmeier et al., 2019; PSNet, 2019). The implication is that infections, especially hospital acquired infections (HAIs) lead to increased length of stay in health facilities, increases susceptibility to other conditions and leads to a rise in medical cost. Imperatively, providers and organizations can leverage innovative approaches like development of EHRs databases to manage data and prevent and reduce the rate of surgical site infections.
Hypothetical EHR Database and Data Required
EHRs are digital forms of patient health information (PHI) and include personal contact data, patient medical history, allergies and treatment plans as well as test and diagnostic results. The benefits of EHRs include improving positive patient outcome and population health, organization and analysis of patient information, and enhancing clinical efficiency through better workflow, timelines, and quality of care. EHRs data can be deployed to create and internally authenticate a data-driven standard to detect at risk patients (Kruse et al., 2018). It also helps in clinical decision support to effectively identify patient at increased risk for surgical site infections. A hospital data management system incorporate all data associated with the facility in an organized manner and is a critical component of EHRs system to enhance interoperability and decision making among providers and patients.
Incorporating Information to Manage the Problem
The EHRs is widely used to gather patient health information including all their details based on the system requirement and are fed into the database. To retrieve information from such a system, one needs to write queries statement with all the criteria needed for its development. The system will offer a multi-tasking functionality by recording patient details while also taking the on duty staff details. The hypothetical database will be created to help colorectal cancer patients. The database will require information collected in the EHRs to input these details automatically. The criteria for data that will be pulled in into the database would include all patients with colon surgical procedure. The additional data would include start and end time of the procedure, room time, gender of the patient, past medical history, weight, family medical history, place of residence, any allergies and previous procedures. The database will also contain the time of medication administration, especially the administration of preoperative antibiotics (De Simone et al., 2018). The goal of these details is to ensure that preoperative antibiotics are administered 30 minutes before the set time for surgical incision.
Patient Problem Incorporating Information Needed
The patient issue being addressed is surgical site infection after a surgical procedure for adult patients with colon or rectal cancer. Surgical site infections (SSIs) after a colorectal procedure are a prevalent issue that impact patient safety and quality care outcomes with numerous reports asserting that close to 25% of such patients get these infections (Coccolini et al., 2018). These infections present a potentially preventable source of mortality, morbidity and resource use in healthcare (Kethman et al., 2019). SSIs are being used increasingly to measure a health care quality status and the main focus of Hospital Acquired Condition Reduction Program (HACRP). The HACRP is a pay-for-performance model that lowers payment to the bottom 25% worst-performing entities in management of surgical site infections and other types of HAIs. The program is focused on enhancing value-based care and paying providers for quality delivered and not quantity.
The pulled information into the database to manage the condition will entail gender, weight and patient past medical history. The database will also have family medical and health history to help in making effective clinical decisions. The data will help providers to determine the susceptibility or risk of the patient for surgical site infections. By pulling these patients into the database using specific information, the providers will ascertain the patients at higher risk for SSI, and give them antibiotics and treat them prophylactically to reduce their vulnerability to infections at the surgical site (Gerson et al., 2019). The implication is that this approach will lead to better health outcomes for the patients.
Data Entities Description
The EHRs implementation leads to collection of vast quantities of data; both structured and unstructured, that providers and facilities need to use to make decisions. Structure data comprises of patient demographics, medications, allergy and vitals, and family history. Structured information pulled in the EHR is easy to evaluate and complete identification of patients at risk for SSIs. Unstructured data comprises of information that does not have a definite model or structural framework. These include medical notes, faxed laboratory results, x-ray images and even patient phone calls (Assale et al., 2019). The information helps clinicians to figure out and obtain more accurate information about a patient’s overall risk for SSIs.
The development of this database will entail pulling data from multiple sources; either as structured or unstructured. However, the database will have mainly structured data as it involves the use of medications before the surgical procedure. The database will have check boxed for past and family medical history, patient age, and patient weight that will be document in pounds. The system will have a drop down for gender with options like male, female and non-binary. Upon the completion of the surgical procedure, the information would be pulled into the database together with the documentation in the operating room done by the anesthesiologist. These would include procedure start and finish time, and time they administered preoperative antibiotic.
The operating surgeon will assess demographics and surgical information for accuracy. The anesthesiologist will assess and validate data on aspects like gender, weight, and body mass index (BMI for accuracy. The implication is that the database will store all associated data that is needed by the facility to make critical decisions to address the issue of SSIs. The system is designed for recording basic details for any facility to reduce SSIs. The current system in most facilities has details about patient ID, name, and address. However, this database will store all information in a structured manner so that the user can easily navigate it based on the system’s requirements.
Conclusion
Through the use of structured data as mentioned in the assignment, facilities can identify with enhanced accuracy, the susceptibility of patients to SSIs. Further, based on this information, they can prophetically medicate them before they develop surgical site infections. SSIs are a significant cause of morbidity, mortality and are associated with not only increased length of stay but also increased rates of readmissions, high costs, and poor patient outcomes. The implication is that there is need to implement practices that will lower the incidences of associated complications and enhance patient safety, quality, and clinical outcomes.
References
Assale, M., Dui, L. G., Cina, A., Seveso, A., & Cabitza, F. (2019). The Revival of the Notes
Field: Leveraging the Unstructured Content in Electronic Health Records. Frontiers in
medicine, 6, 66. https://doi.org/10.3389/fmed.2019.00066
Coccolini, F., Improta, M., Cicuttin, E., Catena, F., Sartelli, M., Bova, R., … & Chiarugi, M.
(2021). Surgical site infection prevention and management in immunocompromised patients: a systematic review of the literature. World Journal of Emergency Surgery, 16(1), 1-13. https://doi.org/10.1186/s13017-021-00375-y
De Simone, B., Sartelli, M., Coccolini, F., Ball, C. G., Brambillasca, P., Chiarugi, M., … &
Catena, F. (2020). Intraoperative surgical site infection control and prevention: a position paper and future addendum to WSES intra-abdominal infections guidelines. World journal of emergency surgery, 15(1), 1-23. DOI: https://doi.org/10.1186/s13017-020-0288-4
Gerson, L., Barton, J., Monaco, C., & Baro, L. (2019). Using EMR to Implement and Track
Compliance of a Unique Colon Bundle That Reduced Surgical Site Infection in Colorectal Surgery: A Single Institution Review. https://digitalcommons.pcom.edu/research_day/research_day_PA_2019/researchPA2019/20/
Grundmeier, R. W., Xiao, R., Ross, R. K., Ramos, M. J., Karavite, D. J., Michel, J. J., … &
Coffin, S. E. (2018). Identifying surgical site infections in electronic health data using predictive models. Journal of the American Medical Informatics Association, 25(9), 1160-1166. https://doi.org/10.1093/jamia/ocy075
Kethman, W., Shelton, E., Kin, C., Morris, A., & Shelton, A. (2019). Effects of colorectal
surgery classification on reported postoperative surgical site infections. Journal of SurgicalResearch, 236, 340-344. https://doi.org/10.1016/j.jss.2018.12.005.
Kruse, C. S., Stein, A., Thomas, H., & Kaur, H. (2018). The use of Electronic Health Records to
Support Population Health: A Systematic Review of the Literature. Journal of medical
systems, 42(11), 214. https://doi.org/10.1007/s10916-018-1075-
Liu, L., Liu, L., Liang, L., Zhu, Z., Wan, X., Dai, H., & Huang, Q. (2018). Impact of
preoperative anemia on perioperative outcomes in patients undergoing elective colorectal surgery.Gastroenterology Research & Practice, 1-7. https://doi.org/10.1155/2018/2417028.
Patient Safety Network (PSNet) (2019 September 7). Surgical Site Infections.
https://psnet.ahrq.gov/primer/surgical-site-infections
