NURS 6630 Study Guide for Medication Treatment Schizophrenia Spectrum and Other Psychosis Disorders
Walden University NURS 6630 Study Guide for Medication Treatment Schizophrenia Spectrum and Other Psychosis Disorders– Step-By-Step Guide
This guide will demonstrate how to complete the Walden University NURS 6630 Study Guide for Medication Treatment Schizophrenia Spectrum and Other Psychosis Disorders assignment based on general principles of academic writing. Here, we will show you the A, B, Cs of completing an academic paper, irrespective of the instructions. After guiding you through what to do, the guide will leave one or two sample essays at the end to highlight the various sections discussed below.
How to Research and Prepare for NURS 6630 Study Guide for Medication Treatment Schizophrenia Spectrum and Other Psychosis Disorders
Whether one passes or fails an academic assignment such as the Walden University NURS 6630 Study Guide for Medication Treatment Schizophrenia Spectrum and Other Psychosis Disorders depends on the preparation done beforehand. The first thing to do once you receive an assignment is to quickly skim through the requirements. Once that is done, start going through the instructions one by one to clearly understand what the instructor wants. The most important thing here is to understand the required format—whether it is APA, MLA, Chicago, etc.
After understanding the requirements of the paper, the next phase is to gather relevant materials. The first place to start the research process is the weekly resources. Go through the resources provided in the instructions to determine which ones fit the assignment. After reviewing the provided resources, use the university library to search for additional resources. After gathering sufficient and necessary resources, you are now ready to start drafting your paper.
How to Write the Introduction for NURS 6630 Study Guide for Medication Treatment Schizophrenia Spectrum and Other Psychosis Disorders
The introduction for the Walden University NURS 6630 Study Guide for Medication Treatment Schizophrenia Spectrum and Other Psychosis Disorders is where you tell the instructor what your paper will encompass. In three to four statements, highlight the important points that will form the basis of your paper. Here, you can include statistics to show the importance of the topic you will be discussing. At the end of the introduction, write a clear purpose statement outlining what exactly will be contained in the paper. This statement will start with “The purpose of this paper…” and then proceed to outline the various sections of the instructions.
Need a high-quality paper urgently?
We can deliver within hours.
How to Write the Body for NURS 6630 Study Guide for Medication Treatment Schizophrenia Spectrum and Other Psychosis Disorders
After the introduction, move into the main part of the NURS 6630 Study Guide for Medication Treatment Schizophrenia Spectrum and Other Psychosis Disorders assignment, which is the body. Given that the paper you will be writing is not experimental, the way you organize the headings and subheadings of your paper is critically important. In some cases, you might have to use more subheadings to properly organize the assignment. The organization will depend on the rubric provided. Carefully examine the rubric, as it will contain all the detailed requirements of the assignment. Sometimes, the rubric will have information that the normal instructions lack.
Another important factor to consider at this point is how to do citations. In-text citations are fundamental as they support the arguments and points you make in the paper. At this point, the resources gathered at the beginning will come in handy. Integrating the ideas of the authors with your own will ensure that you produce a comprehensive paper. Also, follow the given citation format. In most cases, APA 7 is the preferred format for nursing assignments.
How to Write the Conclusion for NURS 6630 Study Guide for Medication Treatment Schizophrenia Spectrum and Other Psychosis Disorders
After completing the main sections, write the conclusion of your paper. The conclusion is a summary of the main points you made in your paper. However, you need to rewrite the points and not simply copy and paste them. By restating the points from each subheading, you will provide a nuanced overview of the assignment to the reader.
How to Format the References List for NURS 6630 Study Guide for Medication Treatment Schizophrenia Spectrum and Other Psychosis Disorders
The very last part of your paper involves listing the sources used in your paper. These sources should be listed in alphabetical order and double-spaced. Additionally, use a hanging indent for each source that appears in this list. Lastly, only the sources cited within the body of the paper should appear here.
Stuck? Let Us Help You
Completing assignments can sometimes be overwhelming, especially with the multitude of academic and personal responsibilities you may have. If you find yourself stuck or unsure at any point in the process, don’t hesitate to reach out for professional assistance. Our assignment writing services are designed to help you achieve your academic goals with ease.
Our team of experienced writers is well-versed in academic writing and familiar with the specific requirements of the NURS 6630 Study Guide for Medication Treatment Schizophrenia Spectrum and Other Psychosis Disorders assignment. We can provide you with personalized support, ensuring your assignment is well-researched, properly formatted, and thoroughly edited. Get a feel of the quality we guarantee – ORDER NOW.
Sample Answer for NURS 6630 Study Guide for Medication Treatment Schizophrenia Spectrum and Other Psychosis Disorders
Schizophrenia is characterized mainly by a clear sensory but a marked thinking disturbance. The psychotic disorder is highly linked with abnormalities of amine neurotransmitter function, especially dopamine. Antipsychotic medications, also called neuroleptic or major tranquilizers, are the first-line drug therapy for schizophrenia. They target the positive symptoms of schizophrenia, like hallucinations, delusions, and disorganized behavior. Antipsychotics act by controlling neurotransmitter dopamine and serotonin levels in the brain. They are classified into two major groups: Typical and Atypical. The antipsychotic effects of Typical antipsychotics owe their competitive blockage to dopamine receptors. Atypicals have fewer extrapyramidal adverse effects than the typical and block both serotonin and dopamine receptors. The purpose of this assignment is to develop a study guide for Risperidone.
Drug Description
- Risperidone is also called Risperdal.
- It is an Atypical neuroleptic medication.
- The FDA approves it for use in the USA in the treatment of:
- Schizophrenia in adults and children aged above 13 years.
- Bipolar I acute manic or mixed episodes as monotherapy in adults and children above 10 years (Álamo, 2022).
- Bipolar I acute manic or mixed episodes adjunctive with lithium or valproate in adults.
- Autism-associated irritability in children above five years.
Off-label uses include:
- Borderline personality disorder
- Delusional disorder
- Delirium
- Depression
- Brain injury
- Pedophilia
- PTSD
- Bipolar disorder
- Conduct disorder
- Lesch-Nyhan
- Tourette Syndrome
- Stuttering, movement disorders
- Developmental disorders
The medication mechanism of action
- Risperidone has a high affinity for serotonin type 2 (5-HT2) receptors.
- It binds to dopamine D2 receptors with 20 times lower affinity than that for 5-HT2 receptors (Zhao et al., 2022).
- It antagonizes alpha1-adrenergic, alpha2-adrenergic, and histaminergic receptors.
- Risperidone has a moderate affinity for serotonin type 1 receptors.
- Has a weak affinity for dopamine D1 receptors.
- No affinity for muscarinic, beta1-adrenergic, and beta2-adrenergic receptors (Zhao et al., 2022).
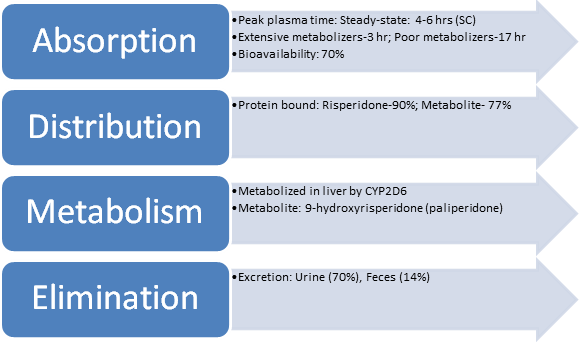
Pharmacokinetics
Pharmacodynamics
- Risperidone decreases dopamine neurotransmission for the five classes of dopamine receptors (D1 to D5).
- It reduces the hallucinations and delusions associated with schizophrenia by blocking dopamine receptors in the brain’s mesolimbic system (Zhao et al., 2022).
Appropriate dosing and administration route,
- Oral: Initial dose at 2 mg/day; Recommended target dosage of 2-8 mg/day OD or BD.
- The oral dose may be increased by 1-2 mg/day at intervals ≥24 hr.
- Intramuscular: 12.5-50 mg into the deltoid or gluteal muscle every 2 weeks; The dose should not be adjusted more often than every 4 weeks.
- Subcutaneous: 90 mg or 120 mg SC once monthly.
Considerations For Dosing Alterations
- Renal Impairment: If Creatine clearance is below 30, PO Risperidone should be initiated at 0.5 mg BD.
- It can be increased by up to 0.5 mg BD to a max of 1.5 mg BD.
Considerations of use and dosing in specific specialty populations
Geriatrics: Lower initial doses are recommended and should be adjusted more gradually.
PO initial dose at 0.5 mg q12hr; IM: 12.5-25 mg (Álamo, 2022).
Pediatrics >13 years: Initiated at lower doses of 0.5 mg/day PO in the morning or evening.
Half-life: This is the time taken for the plasma or blood level of a drug to fall by half.
- Half-life is determined by drug distribution, metabolism, and excretion.
- Half-life is important because drugs that have a short half-life stay in the body for a shorter period and thus have a shorter duration of action (Andrade, 2022).
- Drugs with a short half-life thus need to be administered more frequently.
- Drugs with a long half-life stay longer in the body and thus have a longer duration of action (Andrade, 2022).
- These drugs can conveniently be dosed once a day or less frequently.
- Extensive Risperidone metabolizers have a half-life of 3 hrs (parent and metabolite combined).
- Poor metabolizers have a half-life of 20 hrs (parent and metabolite combined).
Side effects/adverse reaction potentials
- The most significant side effects are Weight gain, metabolic changes, and sedation.
- It is associated with extrapyramidal symptoms (EPS): Acute dystonia, tardive dyskinesia, akathisia, and parkinsonian features (Hodkinson et al., 2021).
- Neuroleptic malignant syndrome (NMS) is a serious side effect of Risperidone.
- Other side effects: Somnolence, Insomnia, Agitation, Anxiety, Headache, Rhinitis, Fatigue, Increased appetite, Vomiting, Drooling, and Urinary incontinence (Hodkinson et al., 2021).

Contraindications for use and drug-to-drug interactions
- Risperidone is contraindicated in patients with known allergy/hypersensitivity to Risperidone or paliperidone (Hodkinson et al., 2021).
- Contraindicated in dementia-related psychosis due to increased risk of death.
Overdose Considerations
- Risperidone overdose is life-threatening.
- Patients with risperidone overdose should be monitored for hypotension, sedation, and respiratory depression.
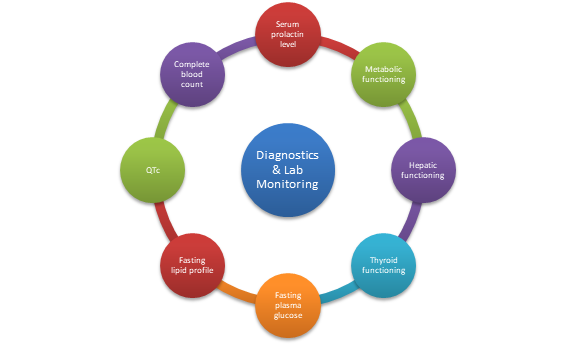
Diagnostics and labs monitoring
- Monitoring plasma concentrations for Risperidone is strongly recommended.
- Monitor for leukopenia/neutropenia and agranulocytosis.
- Monitor complete blood count frequently in the first few months of therapy in patients with a history of low WBC count (Álamo, 2022).
- Specific parameters to be monitored: Serum prolactin level, hepatic functioning, metabolic functioning, thyroid functioning, blood pressure, fasting plasma glucose, fasting lipid profile, and QTc (Álamo, 2022).
Comorbidities considerations
- It should be administered with caution in patients with a history of Parkinson’s disease, Lewy body dementia, seizures, cardiovascular disease, hypovolemia, and dehydration (Álamo, 2022).

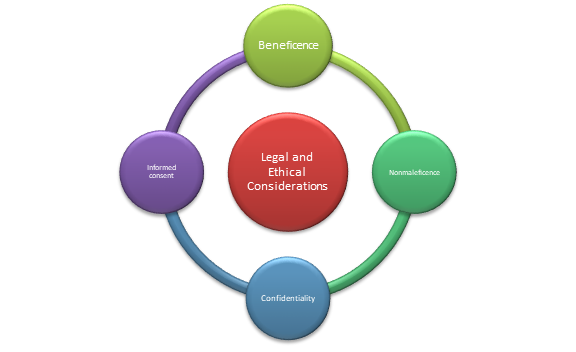
Legal and ethical considerations
- The prescribing clinician should consider legal and ethical factors of beneficence, nonmaleficence, informed consent, and confidentiality when prescribing Risperidone (Hodkinson et al., 2021).
- Beneficence is fostered by prescribing the drug when evidence supports its efficacy and benefits in treating schizophrenia in patients.
- Nonmaleficence is upheld by examining the associated side effects of Risperidone and ensuring the benefits outweigh the possible harm.
- The clinician should obtain consent from the patient by explaining the mechanism of action, benefits, and potential side effects of Risperidone before starting treatment (Hodkinson et al., 2021).
- The clinician should maintain the confidentiality of the patient’s diagnosis and treatment and seek consent before sharing the information with other providers.
Pertinent patient education considerations
- Patient education with regard to Risperidone includes informing the patient of the drug’s benefits in alleviating schizophrenia symptoms and possible side effects.
- Patients should be educated on extrapyramidal symptoms and signs of NMS (Hodkinson et al., 2021).
- They should be instructed on the action to take when serious side effects occur.
Also Read:
WEEK 8 Short Answer Assessment
Assessing and Treating Patients With Sleep Wake Disorders
Assessing and Treating Patients With ADHD
Psychopharmacologic Approaches to Treatment of Psychopathology
Assessing and Treating Patients With Impulsivity, Compulsivity, and Addiction
Conclusion
Risperidone is an Atypical neuroleptic used to treat schizophrenia in adults and children above 13 years. It is also FDA-indicated to treat Bipolar 1 acute manic or mixed episodes and Autism-associated irritability in children above 5 years. It exhibits its therapeutic effects by blocking serotonin and dopamine receptors. The most significant side effects of Risperidone are weight gain, metabolic changes, and sedation. Neuroleptic malignant syndrome and Extrapyramidal symptoms are serious side effects of Risperidone.
References
Álamo, C. (2022). Risperidone ISM as a New Option in the Clinical Management of Schizophrenia: A Narrative Review. Advances in therapy, 39(11), 4875–4891. https://doi.org/10.1007/s12325-022-02299-8
Andrade, C. (2022). The practical importance of half-life in psychopharmacology. The Journal of Clinical Psychiatry, 83(4), 41940. https://doi.org/10.4088/JCP.22f14584
Hodkinson, A., Heneghan, C., Mahtani, K. R., Kontopantelis, E., & Panagioti, M. (2021). Benefits and harms of Risperidone and Paliperidone for treatment of patients with schizophrenia or bipolar disorder: a meta-analysis involving individual participant data and clinical study reports. BMC medicine, 19(1), 195. https://doi.org/10.1186/s12916-021-02062-w
Zhao, M., Ma, J., Li, M., Zhu, W., Zhou, W., Shen, L., Wu, H., Zhang, N., Wu, S., Fu, C., Li, X., Yang, K., Tang, T., Shen, R., He, L., Huai, C., & Qin, S. (2022). Different responses to risperidone treatment in schizophrenia: a multicenter genome-wide association and whole exome sequencing joint study. Translational psychiatry, 12(1), 173. https://doi.org/10.1038/s41398-022-01942-w
Sample Answer 2 for NURS 6630 Study Guide for Medication Treatment Schizophrenia Spectrum and Other Psychosis Disorders
Antipsychotic agents, also called neuroleptic or major tranquilizers, are used primarily to treat schizophrenia. Schizophrenia is characterized primarily by a clear sensory but marked thinking disturbance. Second-generation/ Atypical antipsychotics are widely used due to their broad spectrum of receptor activity since they affect Serotonin, dopamine, and GABA neurotransmitters (de Miranda et al., 2020). Besides, they are better at alleviating negative symptoms and cognitive dysfunction than typical antipsychotics. The purpose of this assignment is to develop a study guide for an antipsychotic agent.
Drug Description
Quetiapine, whose brand name goes by Seroquel, is used in treating schizophrenia. It is FDA-approved for treating schizophrenia, Bipolar disorder, and major depressive disorder (MDD) as an adjunctive treatment (de Miranda et al., 2020).
Non-FDA uses
The non-FDA uses of Seroquel include the treatment of generalized anxiety disorder (GAD), Alcohol Dependence, and Insomnia.
- According to Ansara (2020), Seroquel exhibits efficacy in managing treatment-resistant-GAD as an adjunctive agent. In this case, smaller doses than those prescribed for schizophrenia and bipolar disorder are usually needed for symptom improvement.
- Seroquel has been found to reduce alcohol consumption in heavy drinkers and has the potential for treatment for alcohol dependence, particularly among heavy drinkers (Vatsalya et al., 2020).
- Low doses of quetiapine are usually prescribed for insomnia, although this is a non-FDA use due to potential adverse effects like weight gain and akathisia (Boafo et al., 2020).
Drug classification
Seroquel is an antipsychotic under second-generation antipsychotics.
MOA | Pharmacokinetics | Pharmacodynamics |
An antagonist for D2 receptors and serotonin receptors. | Absorption: Bioavailability: 100% Peak plasma time: Immediate release-1.5 hr; extended release-6 hrs | Reduces the hallucinations and delusions associated with schizophrenia by blocking dopamine receptors in the mesolimbic system of the brain. |
Acts on dopaminergic D1 and D2 receptors. | Metabolism: Metabolized in the liver by CYP3A4 |
|
| Elimination:
Excretion: Urine (73%), feces (20%). |
|
Appropriate dosing: 150-750 mg/day (Immediate release); 400-800 mg/day (extended release).
Children <12 years: safety not established.
Children >12 years: Dose range 400-800 mg/day (de Miranda et al., 2020).
Geriatrics: 50-200 mg/day (Immediate); 50 mg/day (Extended)
Pregnant and breastfeeding women: Not recommended.
Route of Administration: Orally.
Considerations for dosing alterations: Elderly and patients predisposed to hypotensive reactions.
Half-life: The time it takes for the concentration of a drug to decrease to half of its initial dose in the body.
- Understanding half-life is important because it determines a drug’s excretion rates and steady-state concentrations. After one half-life has passed, half of the starting drug amount is eliminated from the body (Smith et al., 2018).
- Seroquel has a half-life of 6 hours for immediate release formulation and 7 hours for extended-release formulation.
Side effects/adverse reaction potentials
Seroquel is associated with various adverse effects, including somnolence fatigue, dry mouth, constipation, increased appetite, weight gain, orthostatic hypertension, and dizziness (de Miranda et al., 2020). Neuroleptic malignant syndrome is a possible adverse effect due to the drug’s D2 receptor blockage.
Contraindications for use including significant drug-to-drug interactions
- Currently, no identified FDA contraindications of quetiapine.
- It is contraindicated in patients with documented hypersensitivity.
- However, quetiapine is associated with an increased risk of death in elderly patients with dementia-related psychosis (Osborne et al., 2020).
- Precaution is needed with drugs that prolong QT intervals and patients with prolonged QT intervals.
Contraindications due to drug-to-drug interactions
- Amisulpride
- Goserelin
- Lefamulin
- Leuprolide
Overdose Considerations
Seroquel can be life-threatening if taken in an overdose. Toxicity occurs with levels > 1500 ng/mL.
Supportive care is the mainstay of treatment in an overdose.
Measures for acute toxicity include: Maintaining the airway; Ensuring adequate oxygenation; Ventilation (Osborne et al., 2020).
Gastric lavage and administration of activated charcoal with a laxative can prevent more drug absorption if promptly given.
Diagnostics and labs monitoring
The prescribing clinician should monitor the patient’s metabolic panel focusing on fasting glucose, cholesterol and triglyceride levels, weight, and blood pressure (before and during treatment). Besides, patients on long-term treatment should have a lens exam every six months for cataract monitoring (Osborne et al., 2020). Leukopenia, neutropenia, and agranulocytosis can occur with Seroquel treatment, and thus a complete blood count (CBC) should be performed during the first few months of treatment (Osborne et al., 2020). In addition, orthostatic vital signs should be monitored in patients vulnerable to hypotension like geriatrics, patients with dehydration, hypovolemia, and those on antihypertensives.
Comorbidities considerations
- Precautions should be taken in patients with hypokalemia, cardiac arrhythmia, and hypomagnesemia. Metabolic panels should be obtained before initiating the drug (Osborne et al., 2020).
- Patients with diabetes mellitus should have their glucose monitored to avoid hyperosmolar coma.
Legal and ethical considerations
- The clinician prescribing Seroquel should uphold beneficence by ensuring that the drug will have the maximum benefit in treating a patient’s psychotic, bipolar, or MDD symptoms. Nonmaleficence should be upheld by considering the drug’s side effects and ensuring that the benefits outweigh the risks.
- The clinician should obtain consent from the patient before initiating treatment with Seroquel and explain the potential benefits and side effects for the patient to make an informed decision.
- Confidentiality of the patient’s health information should be maintained to prevent legal consequences.
Pertinent patient education considerations
The patient should be educated about the drug’s indications, benefits, and side effects. Patients should be informed that the drug can be discontinued if they experience severe side effects and if they have a decrease in WBCs (de Miranda et al., 2020). Besides, they should be educated that abrupt drug discontinuation poses a risk for withdrawal symptoms.
Conclusion
Seroquel is a second-generation antipsychotic, FDA-approved for treating schizophrenia, Bipolar disorder, and MDD. It is also used off-label in treating insomnia, treatment-resistant GAD, and alcohol dependence. Seroquel is an antagonist for D2 receptors and serotonin receptors, which results in reduced psychotic symptoms. Patients on Seroquel should be monitored for cholesterol and triglyceride levels, weight, blood pressure, fasting glucose, cataracts, complete blood count, and orthostatic vital signs. Ethical principles of beneficence, nonmaleficence, confidentiality, and consent should be upheld when prescribing patient Seroquel.
References
Ansara, E. D. (2020). Management of treatment-resistant generalized anxiety disorder. The mental health clinician, 10(6), 326–334. https://doi.org/10.9740/mhc.2020.11.326
Boafo, A., Greenham, S., Sullivan, M., Bazaid, K., Suntharalingam, S., Silbernagel, L., Magner, K., & Robillard, R. (2020). Medications for sleep disturbance in children and adolescents with depression: a survey of Canadian child and adolescent psychiatrists. Child and adolescent psychiatry and mental health, 14, 10. https://doi.org/10.1186/s13034-020-00316-8
de Miranda, A. S., Ferreira, R. N., Teixeira, A. L., & de Miranda, A. S. (2020). Mood Stabilizers: Quetiapine. NeuroPsychopharmacotherapy, 1-23.
Osborne, V., Davies, M., Evans, A., & Shakir, S. (2020). Observational assessment of safety in Seroquel (OASIS): a specialist cohort event monitoring (SCEM) study in England. Therapeutic advances in psychopharmacology, 10, 2045125320954616. https://doi.org/10.1177/2045125320954616
Smith, D. A., Beaumont, K., Maurer, T. S., & Di, L. (2018). Relevance of Half-Life in Drug Design. Journal of medicinal chemistry, 61(10), 4273–4282. https://doi.org/10.1021/acs.jmedchem.7b00969
Vatsalya, V., Kong, M., Marsano, L. M., Kurlawala, Z., Chandras, K. V., Schwandt, M. L., Ramchandani, V. A., & McClain, C. J. (2020). Interaction of Heavy Drinking Patterns and Depression Severity Predicts Efficacy of Quetiapine Fumarate XR in Lowering Alcohol Intake in Alcohol Use Disorder Patients. Substance abuse: research and treatment, 14, 1178221820955185. https://doi.org/10.1177/1178221820955185
NURS 6630 Week 8 Assignment 2 Assessing and Treating Patients With Sleep Wake Disorders
Psychopharmacological approaches to treat psychopathology
Introduction
The patient, in this case, is a 31-year-old man with insomnia. The condition began six months ago after the sudden death of his wife. He is employed as a forklift operator at a local chemical company, but his health condition has affected his ability to perform his work. The patient claims that he has utilized diphenhydramine for sleeping in the past, but he does not like how he feels the next morning after using the medication. According to the patient’s prior physician’s medical record, he was abusing opiates after injuring his ankle in a skiing accident. The patient’s previous physician prescribed him hydrocodone/APAP (acetaminophen) for acute pain management after the accident. For four years, the individual has not received a prescription for an opiate analgesic. He points out that he has recently consumed approximately four beers to help him fall asleep. The patient is attentive and aware of the person talking to him, location, time, and incident. He maintains eye contact and is dressed appropriately for the season. All aspects of judgment, insight, and reality contact remain intact. The man also denies any suicidal ideas and is focused on the future.
Decision One
The treatment should start with Trazodone 10 mg daily at bedtime. Trazodone has been approved as an effective treatment for insomnia. The medicine is effective in lower doses in treating primary and secondary insomnia. Due to its generic availability, the medication is less expensive than newer insomnia medications. Trazodone can also be an effective sleep aid when taken in lower doses. The other reason for selecting the medication is that it is not addictive compared to other insomnia medications such as benzodiazepine class medication such as Valium and Xanax (Yi et al, 2018). The medication can also help the patient improve slow wave sleep, and the medication also has fewer side effects than most of the other medications used in treating insomnia.
There are various reasons why Zolpidem was not selected. The medication can result in severe allergic reactions in some patients. The various signs of allergic reaction due to the medication include swelling of the face and difficulty in breathing. The other reason is that the sedative effect of the medication is stronger than the other available options. The medication can also make a patient experience severe dizziness and drowsiness, resulting in falls, accidents, and severe injuries. Considering the nature of the patient’s work, the medication is not a good option because it can result in daytime drowsiness and dizziness, making the patient not conduct his job effectively. The medication can also result in a high level of aggressiveness and extroversion that is abnormal compared to the patient’s usual behavior (Jung, 2018). Considering that the patient has confirmed that he takes alcohol, Zolpidem cannot be used in the treatment process because the patient can experience auditory and visual hallucinations associated with strange behavior due to alcohol toxicity. Hydroxyzine 50mg was also not selected due to various. One of the main reasons is that the medication has a high side effects profile compared to Trazodone. The medication can also lead to daytime sedation, affecting how the patient will perform at work. Hydroxyzine can also result in various side effects such as skin rash, fast heartbeat, difficulty in swallowing, and chest discomfort (Silvestro, 2021).
From the treatment process, I expect that Trazodone will effectively treat the patient’s condition, and he will be able to sleep well. The patient experience an erection, which will last for approximately 15 minutes as a side effect of the medication. Ethical consideration will positively impact the treatment plan and when communicating with the patient. For instance, every decision and action that I will take will be for the fulfillment of the obligation to provide optimal care to the patient.
Decision Two
Explaining to the patient that an erection that lasts for approximately 15 minutes that he is experiencing is not priapism and should end over time, and he should continue taking the current dose. I choose this decision because the medication effectively treats insomnia, and the patient has enough sleep at night. Continuing with the current dose is also important because the patient is not experiencing any severe side effects apart from the prolonged erections and priapism due to its adrenergic blocking activity.
I did not select the decision to discontinue Trazodone and initiate treatment with suvorexant 1o mg at bedtime daily because of various reasons. Trazodone effectively treated the patient’s condition, and the patient did not experience any side effects; hence, changing the medication will negatively impact the treatment process. Initiating treatment with suvorexant is not a good decision. The medication is associated with various side effects such as next-day drowsiness and agitation. There is also limited evidence supporting the safety of using suvorexant in treating insomnia. The medication can cause the patient to become less alert during the day and feel drowsiness, headache, and dizziness. The medication can also result in memory problems or confusion. The patient can experience disturbed sleep as a side effect and have various experiences such as abnormal dreams, nightmares, and hallucinations. The medication can also cause the patient to experience sleep paralysis or even walk in their sleep.
Decreasing the current trazodone dose to 25 mg daily at bedtime is also not a good decision because the current dose of the medication was effective in treating the patient’s condition. Dose reduction can only be implemented when the patient is experiencing severe side effects due to the medication or it is too expensive for the patient to purchase the current dose of the medication (Yi et al, 2018). Considering the effectiveness of the current dose of Trazodone, reducing the dose can reduce the medication’s efficiency in treating insomnia or slow down the treatment process. I expect the patient to experience a further decrease in priapism from the treatment approach, and insomnia will also decrease. In this case, ethical consideration will ensure that I avoid causing harm to the patient.
Decision Three
The patient should continue with the current dose, and he may split the 50mg tablet into two. Decreasing the dose will help in reducing next-day drowsiness. In order to reduce the side effects of the medication, it is crucial to reduce the current dose to a lower dose considering that the medication is effective and the patient is getting better. Taking a lower dose of Trazodone is proven to be similarly effective than a higher dose, with appreciably fewer adverse effects such as decreased drowsiness and potentially improved quality of life.
The decision to discontinue Trazodone and initiate treatment with sonata 10 mg administered during bedtime is not good. This is because Trazadone has been effective in managing the patient’s condition. Initiating therapy with sonata 10 mg will is not a good decision considering the patient operates a vehicle in the chemical industry. This is because one of the major side effects of the sonata is lack of coordination which can lead to an accident, especially when an individual is driving. Other side effects of the medication that can reduce the patient’s quality of life include dizziness, drowsiness, and short-term memory loss. Another reason why treatment with sonata should not be initiated is that the medication is habit forming and can lead to dependency and can also be abused (Reeve & Bailes, 2010). Due to its habit-forming characteristics, it is not advisable to use the medication in long-term treatment, and it has not been proven to be effective in treating patients with long-term insomnia. Considering the patient has a history of alcohol consumption, the medication is not the best option and can result in various withdrawal symptoms if the patient suddenly stops using it.
The decision to discontinue Trazadone and start treatment with hydroxyzine 50 mg at bedtime is also not advisable. Hydroxyzine cannot be clinically significant to the patient considering the medication has a comparatively long half-life of approximately 20 hours (Schiffman et al, 2011). This will result in daytime sedation after sleeping at night. The medication also has a high side effect profile compared to the low side effect profile of Trazodone. Introducing hydroxyzine can also result in other adverse side effects such as Xerostomia and Xerophthalmia.
From the treatment approach, I expect the patient condition to become better after another four weeks of using the medication. Priapism will also diminish completely, and the level of drowsiness will decrease because the patient will be using a lower dose than the initial dose. Ethical consideration will be crucial in the treatment process and communication with the patient because it will allow me to minimize the medication’s harm to the patient and focus on promoting good health (Haddad, 2018).
References
Haddad, L. M., & Geiger, R. A. (2018). Nursing ethical considerations.
Jaffer, K. Y., Chang, T., Vanle, B., Dang, J., Steiner, A. J., Loera, N., … & Ishak, W. W. (2017). Trazodone for insomnia: a systematic review. Innovations in clinical neuroscience, 14(7-8), 24.
Jung, M. (2018). Zolpidem overdose: a dilemma in mental health. The Health Care Manager, 37(1), 86-89.
Reeve, K., & Bailes, B. (2010). Insomnia in adults: Etiology and management. The journal for nurse practitioners, 6(1), 53-60.
Schiffman, J., Davis, M., Pierre, J., & Saunders, C. S. (2011). Hydroxyzine: rational choice for inpatients with insomnia. Current Psychiatry, 10(3), 88-89.
Silvestro, S. (2021). Hydroxyzine (Vistaril): dosage, uses, side effects. Drugs.
