NRS 415 CLC – Health Care Organization Evaluation
Grand Canyon University NRS 415 CLC – Health Care Organization Evaluation-Step-By-Step Guide
This guide will demonstrate how to complete the Grand Canyon University NRS 415 CLC – Health Care Organization Evaluation assignment based on general principles of academic writing. Here, we will show you the A, B, Cs of completing an academic paper, irrespective of the instructions. After guiding you through what to do, the guide will leave one or two sample essays at the end to highlight the various sections discussed below.
How to Research and Prepare for NRS 415 CLC – Health Care Organization Evaluation
Whether one passes or fails an academic assignment such as the Grand Canyon University NRS 415 CLC – Health Care Organization Evaluation depends on the preparation done beforehand. The first thing to do once you receive an assignment is to quickly skim through the requirements. Once that is done, start going through the instructions one by one to clearly understand what the instructor wants. The most important thing here is to understand the required format—whether it is APA, MLA, Chicago, etc.
After understanding the requirements of the paper, the next phase is to gather relevant materials. The first place to start the research process is the weekly resources. Go through the resources provided in the instructions to determine which ones fit the assignment. After reviewing the provided resources, use the university library to search for additional resources. After gathering sufficient and necessary resources, you are now ready to start drafting your paper.
How to Write the Introduction for NRS 415 CLC – Health Care Organization Evaluation
The introduction for the Grand Canyon University NRS 415 CLC – Health Care Organization Evaluation is where you tell the instructor what your paper will encompass. In three to four statements, highlight the important points that will form the basis of your paper. Here, you can include statistics to show the importance of the topic you will be discussing. At the end of the introduction, write a clear purpose statement outlining what exactly will be contained in the paper. This statement will start with “The purpose of this paper…” and then proceed to outline the various sections of the instructions.
Need a high-quality paper urgently?
We can deliver within hours.
How to Write the Body for NRS 415 CLC – Health Care Organization Evaluation
After the introduction, move into the main part of the NRS 415 CLC – Health Care Organization Evaluation assignment, which is the body. Given that the paper you will be writing is not experimental, the way you organize the headings and subheadings of your paper is critically important. In some cases, you might have to use more subheadings to properly organize the assignment. The organization will depend on the rubric provided. Carefully examine the rubric, as it will contain all the detailed requirements of the assignment. Sometimes, the rubric will have information that the normal instructions lack.
Another important factor to consider at this point is how to do citations. In-text citations are fundamental as they support the arguments and points you make in the paper. At this point, the resources gathered at the beginning will come in handy. Integrating the ideas of the authors with your own will ensure that you produce a comprehensive paper. Also, follow the given citation format. In most cases, APA 7 is the preferred format for nursing assignments.
How to Write the Conclusion for NRS 415 CLC – Health Care Organization Evaluation
After completing the main sections, write the conclusion of your paper. The conclusion is a summary of the main points you made in your paper. However, you need to rewrite the points and not simply copy and paste them. By restating the points from each subheading, you will provide a nuanced overview of the assignment to the reader.
How to Format the References List for NRS 415 CLC – Health Care Organization Evaluation
The very last part of your paper involves listing the sources used in your paper. These sources should be listed in alphabetical order and double-spaced. Additionally, use a hanging indent for each source that appears in this list. Lastly, only the sources cited within the body of the paper should appear here.
Stuck? Let Us Help You
Completing assignments can sometimes be overwhelming, especially with the multitude of academic and personal responsibilities you may have. If you find yourself stuck or unsure at any point in the process, don’t hesitate to reach out for professional assistance. Our assignment writing services are designed to help you achieve your academic goals with ease.
Our team of experienced writers is well-versed in academic writing and familiar with the specific requirements of the NRS 415 CLC – Health Care Organization Evaluation assignment. We can provide you with personalized support, ensuring your assignment is well-researched, properly formatted, and thoroughly edited. Get a feel of the quality we guarantee – ORDER NOW.
Sample Answer for NRS 415 CLC – Health Care Organization Evaluation
Importance of inter-professional collaboration for Healthcare Organizations’ Culture and values
Inter-professional collaboration is a core aspect of effective working in any healthcare setting, including the University of California Care, UC Care hospital as the entails different healthcare professional from diverse fields working together to deliver care. Inter-professional collaboration ensures that providers, especially nurses and physicians work through teams to deliver patient care (Rider et al., 2021). Through teamwork, the professionals work together, share knowledge and learn from one another. The collaboration promotes patient-centered care culture as the professionals develop a common approach to patient care. Such plans address all areas of patient health and integrates evidence-based practice (EBP) to improve quality delivery. Through inter-professional collaboration, organizations and the professionals develop a continuous learning culture that encourages gaining of new knowledge and skills to improve patient care (Borkowski et al., 2020). Trust and mutual respect also develop as collaboration enhances the connections among healthcare workers as the disciplines work together. The professionals develop a culture of transparency, shared learning and decisions and appreciation of diverse view and opinions. The culture of respect emerges and endures as providers listen to one another.
Importance of Shared Governance on organizational culture and values
Shared governance entails participating in decisions concerning patient care, quality improvement, and guidelines within an organization. Shared governance provides a voice or platform for employees to determine the organizational culture, values and processes. Through shared governance, providers and organizations cooperate and communicate effectively to attain set goals and objectives (Wei et al., 2020). For instance, open communication fosters a culture based on tolerance, mutual respect, and shared accountability where everyone takes responsibility for decisions and actions at both individual and organizational levels. Shared government leads to empowerment and ownership as employees feel part of the organization based on their decisions and input (Borkowski et al., 2020). The providers also share decision-making and develop care plans for better access and quality care.
Inter-professional collaboration and Shared Governance at University of California Care-UC Care-UCnet
Inter-professional collaboration and shared governance are core aspects of care delivery at University of California Health- UC Care since the facility has professionals from diverse fields and specialties who cater to its patients or clients. These professionals work together through the organization to deliver quality patient care. The professionals are practitioners in different areas of care but make collective decisions and develop requisite care plans for their patients. The practitioners at UC Care develop care plans through multidisciplinary teams implying that inter-professional collaboration will be critical (UC, 2024). The use of different programs and plans like Medicare implores the organization to leverage inter-professional collaboration to improve care delivery and communication among the different players (Rider et al., 2021). Lastly, UC Care requires shared governance and inter-professional collaboration because it deals with diverse patients, particularly the elderly who are susceptible to commodities.
ALSO READ:
NRS 415 Professional Accountability Reflection
NRS 415 Benchmark – Creating Change Through Advocacy
NRS 415 Benchmark – Applying Leadership and Management Principles
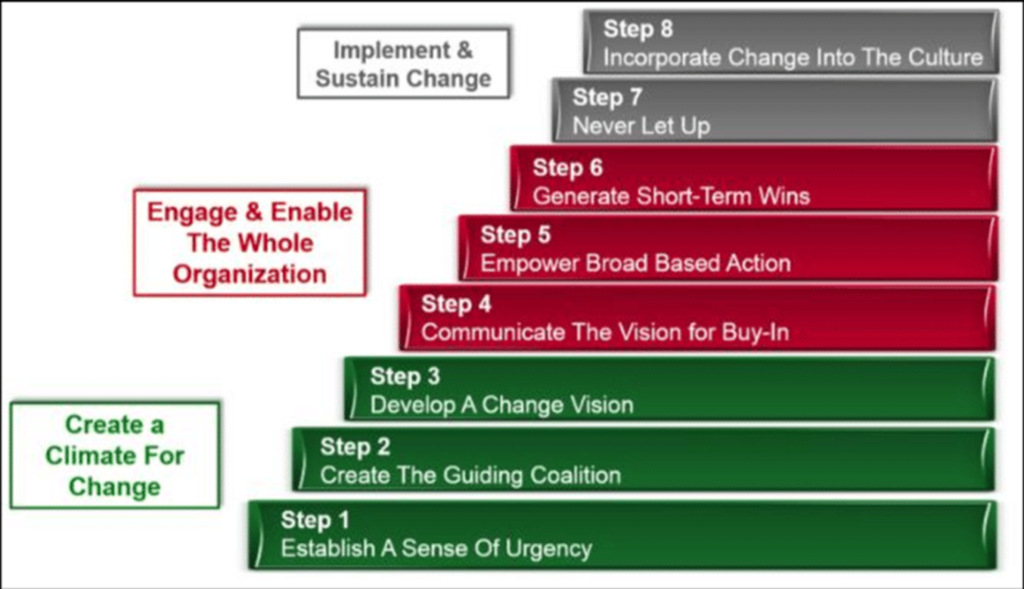
Change Management Theory: Kotter’s 8-Step Change Model
The appropriate change management model for the organization as it navigates its strategic plan is Kotter’s 8-step model. The model is systematic in implementing change in organizations, including healthcare entities like UC Care. The change process requires urgency and a coalition of change agents who will embrace the developed change vision of the leader. The process also entails communicating the vision for all stakeholders to accept or have a buy-in. The fifth step is to empower broad-based action across the organization based on the strategic plan (Borkowskie et al., 2020). For instance, UC Care’s strategic plan is to expand its services to cater to more populations based on the unique patient needs. The sixth step is generation of short-term wins like departmental implementation before implementation in other areas. The seventh step is to build on the short-term wins by developing new plans based on commitment from the employees. The eighth or final step is anchoring change as part of the organizational culture through persistency and better approaches for employees to leverage the new ways of doing things.
Why the Model is Appropriate
Kotter’s 8-step change model is appropriate for this organization based on its attributes and structure. The model is systematic yet broad based on its steps. The implication is that at any level, the model integrates all stakeholders in an organization based on their roles and responsibilities. The eight-step process ensures that stakeholders generate a buy-in or acceptance as it entails communicating the planned changes and integrating all concerned (Wei et al., 2021). The eight-step process is also important for UC Care since it emphasizes effective communication as a core aspect of change implementation. The implication is that this change model acknowledges the important role that people play in change management, especially their input and participation in decision-making.
References
vBorkowski, N., & Meese, K. A. (2020). Organizational behavior in health care.
Jones & Bartlett Learning.
vRider, E. A., Frost, J. S., & Longmaid III, H. E. (2021). Embedding shared
inter-professional values in healthcare organizational culture: The National
Academies of Practice experience. Journal of Inter-professional Education &
Practice, 23, 100348. DOI:10.1016/j.xjep.2020.100348
vUniversity of California Health (UC Care) (2024). About Us: Committed to the
health and well-being of all. https://health.universityofcalifornia.edu/about-us
vWei, H., Corbett, R. W., Ray, J., & Wei, T. L. (2020). A culture of caring: the
essence of healthcare inter-professional collaboration. Journal of inter-
professional care, 34(3), 324-331. DOI: 10.1080/13561820.2019.1641476.
Sample Answer 2 for NRS 415 CLC – Health Care Organization Evaluation
Overall Readiness to Improve Care Outcomes 1 of 3
Providence strives to create change and improve patient outcome by acknowledging issues and coming up with strategies to create changes. Providence is open with their plans of improvement and posts their improvement plans on their website. Improvement plans are created for each facility because each facility has their own weaknesses and strengths that must be acknowledged. Improvement plans focus heavily on community resources and collaboration with others to help provide best care for patients.
Overall Readiness to Improve Care Outcomes 2 of 3
#2- Min Ji -Describe the organization’s overall readiness to improve care outcomes based on your findings.
Providence Hospital Mission (Mission Viejo and Laguna Beach) are the 2 Mission organizations closest to me so I chose these facilities to focus on. Improved patient outcome is divided into 2 major ways for Providence organization. One way of improving patient care outcome is community needs and another is improvements that can be made within the hospitals. This slide focuses on community care and needs being addressed. Providence believes that patient care isn’t only in hospital setting but also outside the hospital as well. That is why in order to improve care, they utilize community hearings identify improvements needed. Providence takes both inputs from listening sessions along with surveys to see where their priorities need to be and offer strategies to create these improvements. The improvement plan has not been posted for the 2024-2026, but for the improvement plan for 2021-2023, improvements included mental health challenges and access to healthcare. Providence’s plans to improve these issues of care included community programs, services that can be offered and low cost resources (2021-2023 community health- providence, n.d.).
Overall Readiness to Improve Care Outcomes 3 of 3
#2- Min Ji -Describe the organization’s overall readiness to improve care outcomes based on your findings.
Providence utilizes CORE to analyze and collect data to see where improvements can be made. CORE utilizes data to identify improvements anywhere from management changes to changes in how physical care to patient is given. CORE looks at data more involved with hospital setting, although it also does look at community changes. By utilizing CORE, Providence acknowledges that there is room for improvements and looks to actively make changes for the better.
Introduction
Providence Health & Services launched its Mission: Forward strategic plan in 2019, addressing network growth, nurse staffing, resource management, and patient satisfaction. The plan has been adjusted to reflect current issues, challenges, and opportunities in healthcare, ensuring a well-planned approach to healthcare.
Strategic Plan Analysis
Under Don Antonucci’s leadership, the organization has strategically pursued network growth through dynamic partnerships with various groups, including Virta Health, Kaia Health, and Cigna. The organization also uses its integrated system and technology to increase members’ access.
Proper nurse staffing is crucial for better health outcomes and patient satisfaction (Cho et al., 2020). Providence House plans to ensure an adequate number and skilled mix of patient care staff. The organization has added four new staff members to its growing team in 2022-2023.
Resource management is crucial for the distribution of healthcare professionals. The organization is aware of inflation-related issues, such as heating buildings and hiring new staff (Mousa & Othman, 2020). To address these issues, the organization plans to restructure managerial roles and relaunch Silver Lining House as a peer-based program for young single men.
To increase patient satisfaction, the organization plans to use technology integration, such as a patient engagement platform launched within Renton. This platform connects fragmented data sources and point solutions, creating better patient experiences.
Conclusion
In conclusion, the Mission: The initiative followed by Providence Health & Services is an example of a strategic plan that includes network growth, nurse staffing, resource management, and patient satisfaction. The facility leadership uses mutable alliances to develop a broad approach to networking; new members are joined as an expression of commitment towards nurse staffing. In the strategic restructuring of resource management challenges related to inflation, the organization seeks technological integration to enhance patient satisfaction.
Conflict within Interprofessional Collaboration
#4- Kate
1.Examine how interprofessional collaboration and shared governance influence organizational culture and values.
Change Model for Providence’s Strategic Plan: Kotter’s Change Theory
#5-Regina
Change implementation models are essential when executing transformation in organizations, including Providence Health. Change models provide guidelines on ways to implement new ways of doing things in a healthcare organization to improve service provision and care delivery (Campbell et al., 2020). The selected change model or theory is Kotter’s change model. The model is a middle-range framework to manage change as it can be tested empirically, distinguishing it from grand theories. According to Kotter, change entails both emotional and situational components (Mohiuddin et al., 2020). The model comprises eight-step process aimed at transitioning individuals from one identity to a new one during the process.
Stages of Kotter’s Change Model
#5- Regina
At the core of this model is effective implementation of change by organizational leaders. They attain change or transformation by improving the organizational culture and motivating employees, nurses, to contribute to quality improvement. Through engaging employees in the change process, the theory ensures acceptance of the transformation and enhance the success of the quality improvement process (Harrison et al., 2021). Kotter’s change theory entails eight steps that enable healthcare organizations and their leaders to implement change. These include creating a sense of urgency or demonstrating the need for change, creating s coalition or team to lead and guide the change, developing and sharing a vision for change, and communicate the vision to the employees. The fifth step is to empower employees to implement the developed vision for the organization (Mohiuddin et al., 2020). The sixth step is to implement quick actions aimed at attaining quick wins based on the developed vision. The seventh step is to build on the change based on quick wins while the eighth step is to make the changes part of the organizational culture and processes. For instance, the healthcare organization will make the new changes part of its systems for better care services delivery.
Significance of the Change Model
Kotter’s change model is one of the most prevalent models in change management. The model is appropriate for the organization as it allows stakeholders to adapt to changes in a systematic manner. The model helps the organization to empower its employees to attain effective changes in their processes and procedures. It also enhances unity to improve the quality of care by following each step (Harrison et al 2021). The model is appropriate since it improves organizational as it requires entities to employ the new practices and motivate employees to implement them to change care delivery. The model offers an evidence-based practice approach for enhanced care delivery Campbell et al., 2020). Kotter’s eight-step model assists healthcare leaders to implement change in a strategic manner for better care delivery in org.
References
Livet, M., Blanchard, C., & Richard, C. (2022). Readiness as a precursor of early implementation outcomes: an exploratory study in specialty clinics.
Implementation science communications, 3(1), 94. https://doi.org/10.1186/s43058-022-00336-9
Nagle, K. (n.d.). Organizational behavior. 10.3 Causes and Outcomes of Conflict| Organizational Behavior.
https://courses.lumenlearning.com/suny-orgbehavior/chapter/10-3-causes-and-outcomes-of-conflict/
- Mousa, S. K., & Othman, M. (2020). The impact of green human resource management practices on sustainable performance in healthcare organisations: A conceptual framework. Journal of cleaner production, 243, 118595.
2021 – 2023 community health – providence. (n.d.).
https://www.providence.org/-/media/Project/psjh/providence/socal/Files/about/community-benefit/reports/missionviejolagunabeach2021-2023chip.pdf?la=en&hash=B04282B06C92847B58B70D2090CF9C40
Campbell, R. J. (2020). Change Management in Health Care. Healthcare
Management, 39(2):50-65.DOI: 10.1097/HCM.0000000000000290.
Harrison, R., Fischer, S., Walpola, R. L., Chauhan, A., Babalola, T., Mears,
S., & Le-Dao, H. (2021). Where do models for change management,
improvement and implementation meet? A systematic review of the
applications of change management models in healthcare. Journal
of healthcare leadership, 85-108. doi:10.1136/leader-2020-000379
Mohiuddin, S., & Mohteshamuddin, K. (2020). Combination model for
sustainable change by utilizing the Kotter’s change model and the
Hersey & Blanchard’s leadership model for improving medication
errors reporting. Journal of Medical & Allied Sciences, 10(1), 25-32.
DOI: 10.5455/jmas.76372
